Macula & Retina Specialist
Associate Professor Hemal Mehta
Dr Mehta is an expert in the diagnosis and management of macula and retinal disease, with over a decade of experience managing thousands of patients at leading centres in Sydney and London. Dr Mehta takes the time to explain the diagnosis, discuss management options and answer any questions patients or relatives may have.
Dr Mehta has published extensively on the management of macula disease, including use of the latest intravitreal and laser therapies. He has helped the Macular Society develop educational material for patients and carers. Dr Mehta was awarded the Royal College of Ophthalmologists Ethicon Award to support streamlining of diabetic retinopathy screening in the Northern Territory. He is on the Steering Committee of the Fight Retinal Blindness! registry that audits real-world outcomes of intravitreal therapy for conditions like wet age-related macular degeneration to optimise patient care.

Age-related macular degeneration (AMD)
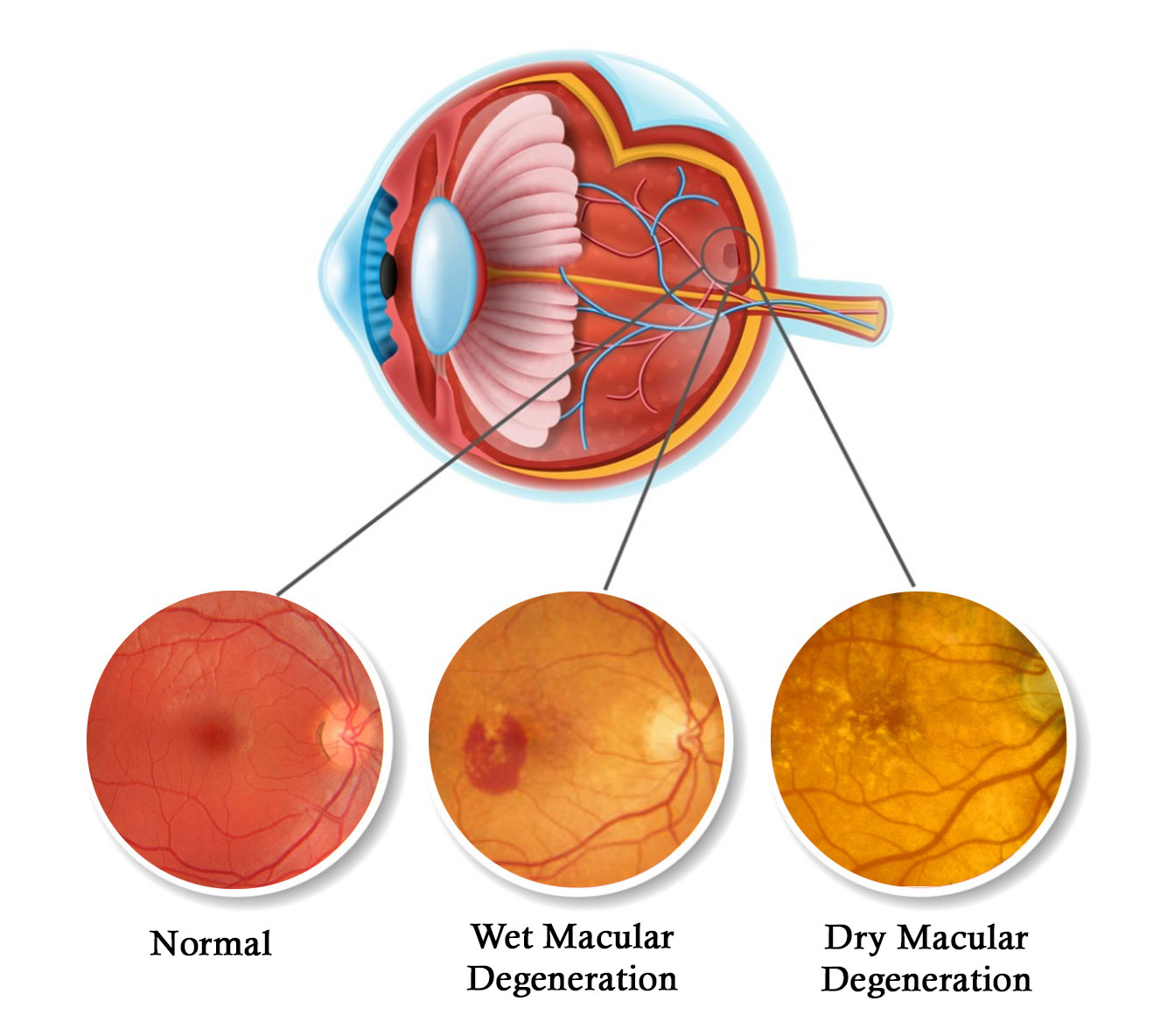
Wet age-related macular degeneration
Wet AMD leads to rapid deterioration in the central vision without treatment. It is called ‘wet’ because of the leakage and build-up of fluid that occurs at the macula (central retina) with this disease. The peripheral or navigational vision is usually not affected. The disease becomes progressively more common with age.
Symptoms include waviness of straight lines, decreased central vision, or an area of the central vision missing. An Amsler Grid like the one available for download below, can be used to monitor for these symptoms. With the advent of intravitreal anti-VEGF therapy, it is now possible to stabilise and sometimes initially improve the vision. The earlier the disease is identified and treatment commenced, the better the long-term visual outcome. Maintenance of therapy is usually required long-term to maintain the vision.
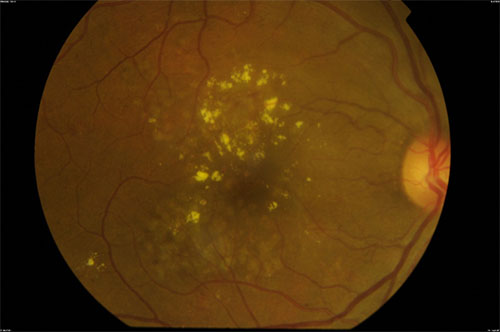
Dry age-related macular degeneration
Dry AMD describes the more gradual wear and tear changes at the macula that gradually develop over many years. This gradually causes the central vision to deteriorate. There is not currently a licensed treatment to reverse the dry AMD changes.
Lifestyle measures aim to slow the progression to late AMD. These include quitting smoking, a balanced diet with plenty of green leafy vegetables and wearing sunglasses with UV protection in direct sunlight. Vitamin supplements consistent with the AREDS2 formulation can also be considered.
Magnifiers and additional lighting can help with reading tasks when the AMD is more advanced.
Diabetic retinopathy
Diabetic macula oedema (DMO)
Diabetes can damage blood vessels at the centre of the vision leading to leakage of fluid in the macula causing blurred central vision. The most important risk factors are high blood sugars and high blood pressure.
As well as optimising overall diabetic control and lifestyle measures, eye treatment can be required. For non-centre involving DMO, focal macular laser can be considered. For mild centre-involving DMO, micropulse laser is an option. For significant centre-involving DMO, intravitreal therapy is the gold standard for the best visual outcomes.
Proliferative diabetic retinopathy

Diabetic retinopathy can lead to the development of new blood vessels at the back of the eyes (proliferative diabetic retinopathy). These new blood vessels are fragile and can bleed in the eyes (vitreous haemorrhage) leading to severe visual loss.
Sometimes surgery is required to clear the vitreous haemorrhage and traction on the retina. It is best to identify new blood vessels before vitreous haemorrhage develops. There may be no visual symptoms at this stage. Hence, the need for regular diabetic retinopathy screening. Panretinal photocoagulation laser treatment can be used to reduce the risk of vitreous haemorrhage in the long-term. Intravitreal anti-VEGF therapy can be a useful short-term measure to reduce the risk of vitreous haemorrhage.
Central serous retinopathy
Central serous retinopathy (CSR) describes a condition where fluid develops in the central vision (macula) in patients of working age. It is more common but not exclusive to males. Symptoms can include blurred central vision, washing out of colours and waviness of straight lines. Steroids play an important role. This can either be external steroids in the form of steroid tablets, nasal sprays or creams or internal production of steroid (cortisol), usually due to stress.
On one end of the spectrum, is acute CSR which usually resolves within 6 months, especially when the trigger is removed. Patients often have recurrent episodes. On the other end of the spectrum, is chronic CSR which can cause significant long-term damage to the central vision and does not resolve without intervention.
CSR is now recognised to be on a spectrum of choroidal diseases called the ‘pachychoroid diseases’. Diagnostic tools available in specialist retinal clinics including fluorescein, indocyanine green and OCT angiography can help diagnosis and planning of treatment.
There can be benefit from lifestyle measures like reducing stress or improving sleep patterns as well as avoiding steroid-based medications. If required, interventions include oral medications to reduce steroid levels, micropulse laser, photodynamic (cold) laser therapy, or intravitreal anti-VEGF therapy.
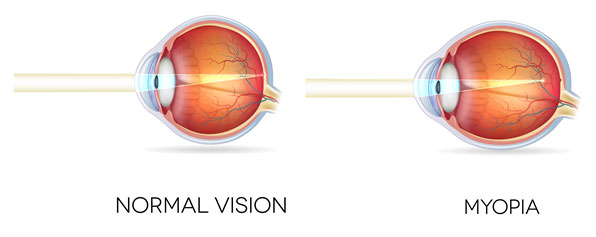
Pathological myopia
Being short sighted (myopic) is associated with wearing glasses or contact lenses to improve distance vision. There are other potential implications of myopia, mainly affecting the back of the eye. Myopia is becoming increasingly common and tends to cause retinal complications in working-age individuals. These complications include retinal detachment, wear and tear changes in the central vision and leakage of blood vessels at the centre of the vision.
Retinal detachment
Individuals with myopia have larger eyeballs and the retina is therefore thinner than those without myopia. This increases the rate of high-risk retinal holes and retinal tears in patients with myopia. Untreated, these can act as a gateway for fluid to track under the retina causing a detachment. Retinal detachment can lead to significant visual loss, especially if the central part of the retina (the macula) detaches. Barrier laser around retinal breaks can reduce the risk of retinal detachment developing.
Myopic macular atrophy
Wear and tear changes can gradually develop in the central vision of patients with myopia. This is similar to dry age-related macular degeneration but tends to occur in a younger age-group. Currently, treatments are not available to reverse these atrophic changes. Additional lighting and magnification can help with reading tasks.
Myopic choroidal neovascularisation (CNV)
Because the barrier layer that separates the retina from the rich supply of blood vessels next to it is thin in myopia, it is possible for blood vessels to break into the central part of the retina (macula) and cause leakage and bleeding. Similar to wet age-related macular degeneration, this can lead to symptoms including waviness of straight lines, decreased central vision, or an area of the central vision missing. An Amsler grid, like the one available for download here, can be used to monitor for these symptoms. With intravitreal anti-VEGF therapy, it is possible to stabilise and sometimes improve the vision. The earlier the disease is identified and treatment commenced, the better the long-term visual outcome. Usually, continuous long-term intravitreal anti-VEGF treatment is not required.
Retinal tears and holes
Retinal detachment can lead to significant visual loss, especially if the central part of the retina (the macula) detaches, and requires surgery to help improve the vision. Usually, retinal tears or high-risk retinal holes develop first. There is the opportunity to intervene with barrier retinal laser at this stage in a clinic setting to prevent fluid tracking under these retinal breaks and reduce the risk of retinal detachment formation.
Retinal tears can develop when the vitreous jelly separates from the back of the eye (posterior vitreous detachment). The vitreous jelly separates at a younger age in myopic individuals. Symptoms typically include a dramatic increase in floaters, flashing lights that persist or an area of the peripheral vision that is completely blacked out. If these symptoms develop, it is important to have an urgent ophthalmology assessment.
Retinal holes can develop in eyes that are myopic or had trauma. In the early stages, they often do not cause visual symptoms. If fluid tracks through the hole and gradually detaches the retina, patients can report symptoms of flashing lights or an area of the peripheral vision that is completely blacked out. The vitreous jelly does not have to separate for this kind of retinal detachment to develop. If you notice these symptoms, it is important to have an urgent ophthalmology assessment.
Retinal vein occlusions
Retinal vein occlusions usually occur in patients over the age of 50 years with high blood pressure or diabetes. They can also occur in younger patients where an issue with blood flow or clotting may be the underlying cause. Therefore, as well as managing the eye disease, a physician is usually involved to try and identify and treat the underyling disease.
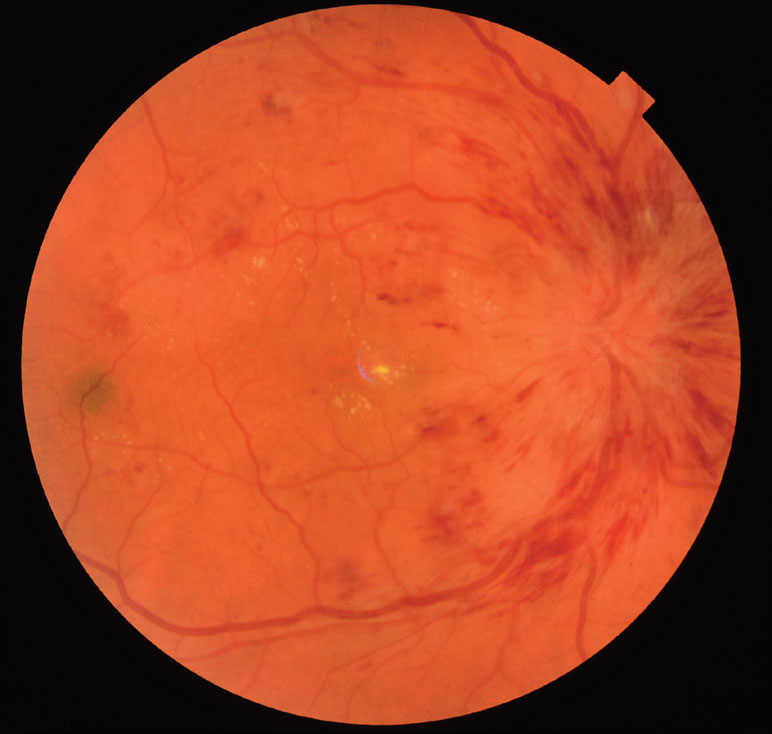
Central retinal vein occlusion (CRVO) occurs when entire retinal vein is blocked as it enters the eye at the optic nerve head. There can be a wide range of presentations from mild disease to very severe sight-threatening disease. There can be a build-up of fluid at the centre of the retina, called cystoid macular oedema which can cause waviness of straight lines or blurred central vision. Intravitreal therapy can help to dry this fluid and improve central vision. The CRVO can also impair the blood supply to the central vision, macular ischaemia, which can limit how much vision can be regained. There can also be development of new blood vessels at the front of the eye, leading to the eye pressure becoming elevated (rubeotic glaucoma) and the eye becoming painful. Retinal laser treatment can reduce the risk of rubeotic glaucoma developing.
Branch retinal vein occlusion (BRVO) describes when one of the major retinal veins becomes blocked. If the blocked retinal branch supplies the macula, then fluid can build-up (cystoid macular oedema). Symptoms typically include waviness of straight lines or blurred central vision. Intravitreal therapy can help to dry this fluid and improve central vision. The BRVO can also impair the blood supply to the central vision, macular ischaemia, which can limit how much vision can be regained. There can also be development of new blood vessels at the back of the eye which are fragile and can easily bleed into the vitreous jelly of the eye. Retinal laser can be targeted to areas of the retina with poor blood supply (ischaemia) to reduce this risk.
Any surgical or invasive procedure carries risks. The information provided here is for general educational purposes only. For more information on macula and retina surgery in your situation, please contact Dr Mehta's rooms.
Associate Professor
Hemal Mehta
MBBS MD(Cantab.) FRCOphth FRANZCO
Strathfield Retina
STRATHFIELD
Eastern Suburbs Eye Specialists
BONDI JUNCTION
Norwest Eye Clinic
BELLA VISTA
Central Coast Eye Specialists
GOSFORD & LONG JETTY